November 19, 2024 | Black & Kletz Allergy
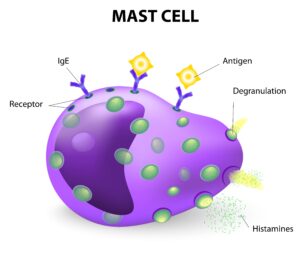
Mast cell activation syndrome (MCAS) has been a hot topic in recent years. It seems as though the prevalence is increasing over the last decade. Mast cell activation syndrome is caused by episodes of the abnormal release of mast cell mediators which can affect any organ system, but tends to involve the skin, nervous system, cardiovascular system, and gastrointestinal tract mostly. Before delving into the syndrome, it is important to understand the science behind it.
The symptoms an individual with mast cell activation syndrome experiences depends on where the mast cells are degranulating. In general, children are more likely to have dermatologic symptoms whereas adults tend to have symptoms related to other organ systems as well as the skin. The symptoms associated with the skin may include generalized itching, flushing, hives and/or swelling. Gastrointestinal symptoms may include abdominal bloating, abdominal pain, throat tightness, nausea, vomiting, and/or diarrhea. A patient may exhibit respiratory problems such as coughing, wheezing, shortness of breath, and/or chest tightness. There may be cardiovascular symptoms such as decreased blood pressure, fainting (syncope), lightheadedness, and/or increased heart rate (i.e., palpitations). Neurological manifestations may cause “brain fog,” fatigue, headaches, sleep disturbances, and/or inability to concentrate. If the bone marrow is involved, fractures, bone pain, and anemia may ensue. The lymphatic system may be involved, thus causing swelling of lymph nodes, spleen, liver, and other organs.
There is evidence that mast cell activation can be associated with postural orthostatic tachycardia syndrome (POTS). Postural orthostatic tachycardia syndrome is a condition where one’s pulse rate increases by a substantial amount, usually greater than 30 beats per minute) upon standing or sitting up.
There is also evidence that mast cell activation can be associated with connective tissue diseases such as hypermobile type of Ehlers-Danlos syndrome (hEDS). A proportion of individuals with the hypermobile type of Ehlers-Danlos syndrome also have mast cell activation syndrome, leading to the possibility of a link between the 2 conditions. In one study, 66% of patients with both a high heart rate when standing [i.e., postural orthostatic tachycardia syndrome (POTS)] and Ehlers-Danlos syndrome also had symptoms consistent mast cell activation syndrome.
Sometimes mast cells become defective and release mediators because of abnormal internal signals. Certain mutations in mast cells can produce populations of identical mast cells (i.e., clones) that overproduce and release more chemical mediators. These abnormal clones can grow uncontrollably and are quite sensitive to mast cell activation. Individuals with this condition are said to have a disorder referred to as mastocytosis. Mastocytosis can be further divided into 2 subgroups: cutaneous mastocytosis and systemic mastocytosis.
Cutaneous mastocytosis only affects the skin and is more common in children. It is defined by red or brown itchy lesions on the skin. The most common type of cutaneous mastocytosis is called urticaria pigmentosa.
Systemic mastocytosis affects other parts of the body besides the skin such as lymph nodes, bone marrow, stomach, intestines, liver, and spleen. Very rarely however, mast cell leukemia or mast cell sarcoma can occur in patients with systemic mastocytosis.
The diagnosis of mast cell activation syndrome is somewhat difficult in many patients. Increases in the chemical mediator tryptase may be found in the blood, but normal levels of tryptase does not rule out the diagnosis. Tryptase should be drawn between 30 minutes and 2 hours after the beginning of an episode, with a baseline level obtained many days later. In addition to serum tryptase, elevated 24 hour urine levels of N-methylhistamine, 11B -prostaglandin F2α (11B-PGF2α), and/or leukotriene E4 (LTE4) are useful tests in the diagnosis of mast cell activation syndrome.
The treatment of mast cell activation syndrome should aim to relieve the annoying symptoms that many find maddening. H1-blocking antihistamines are effective in reducing many of the symptoms in some individuals. H-2 blockers may work in conjunction with the H1 antihistamines to give better relief. Leukotriene antagonists [i.e., Singulair (montelukast), Accolate (zafirlukast), Zyflo (zileuton) may also offer additional help in alleviating unwanted symptoms. These leukotriene antagonists help by blocking the effects of leukotriene C4 (LTC4) or 5-lipoxygenase (5-LPO), depending on the leukotriene antagonist used. Mast cell stabilizers (i.e., cromolyn sodium) may be useful in that they stabile mast cell membranes, thus reducing degranulation, and causing less of the chemical mediators to be released into the tissues. Aspirin and NSAID’s (nonsteroidal anti-inflammatory agents) have a role in treatment, particularly of flushing, as they block the production of the chemical mediator prostaglandin D2 (PGD2). In recalcitr carry a self-injectable epinephrine device (i.e., EpiPen, Auvi-Q, Adrenaclick)) or Neffy, an epinephrine containing nasal spray, as a precaution. If the epinephrine is used by the patient, the individual should then go to the closest emergency room. Although not FDA-approved to treat mast cell activation syndrome, Xolair (i.e., omalizumab), a monoclonal antibody that blocks the binding of the IgE molecules to its receptors, has been reported to reduce mast cell reactivity and sensitivity to activation which can reduce anaphylactic episodes.
The board certified allergy specialists at Black & Kletz Allergy treat both adult and pediatric patients. We have offices in Washington, DC, McLean, VA (Tysons Corner, VA), and Manassas, VA. All 3 of our offices have on-site parking. The Washington, DC and McLean, VA offices are Metro accessible and the McLean, VA office has a free shuttle that runs between our office and the Spring Hill metro station on the silver line. You may also click Request an Appointment and we will respond within 24 hours by the next business day. Black & Kletz Allergy has been a fixture in the greater Washington, DC, Northern Virginia, and Maryland metropolitan community for over 50 years for our outstanding services for the diagnosis and treatment of mast cell activation syndrome, allergic rhinitis (hay fever), asthma, eczema (atopic dermatitis), insect sting allergies, food allergies, medication allergies, hives (urticaria), swelling episodes (angioedema), contact dermatitis, eosinophilic disorders, and immunological conditions.












